In the summer of 2023, members of the Washtenaw Health Initiative’s Communications Committee sat down to discuss the challenges posed by Michigan’s Medicaid redetermination process, including the growing number of Michiganders losing coverage each month.
With leadership from staff and administrators at the Washtenaw Health Project, the committee crafted 12 recommendations to streamline the process and minimize unnecessary insurance losses. These suggestions include simplifying paperwork, sharing alternative coverage options, improving telephonic support, enhancing report data, and more. The recommendations were endorsed by a number of WHI member organizations and shared with key staff at the Michigan Department of Health and Human Services.
“Our staff, MDHHS and so many people are working hard to make sure as many people have healthcare coverage as possible,” says Jeremy Lapedis, executive director of the Washtenaw Health Project. However, there is still so much more that we can do to make accessing coverage easier, so people can get the healthcare and medications they need to stay healthy and be financially protected from medical debt
As of January, 2024, recommendations 2 and 5* have been implemented in Michigan. Washtenaw Health Project leaders have met with key staff at the Michigan Department of Health and Human Services to discuss challenges to the redetermination process and steps the state is taking, or could take, to improve the process. They will continue to do so for the foreseeable future.
If you’d like to share your thoughts regarding Michigan’s Medicaid redetermination process, you can reach out to your Michigan Senate and House representatives.
| 1. | Simplify paperwork. Many Medicaid enrollees have tried to complete the state’s renewal materials, but have found the instructions difficult to follow. The renewal form, in particular, is unnecessarily long and complicated. Simplify paperwork, particularly the renewal form, and provide translations for non-native English speakers. |
| 2. | Provide blank forms.* Currently, renewal forms are only available through mailings, MiBridges, and DHS locations. Blank forms should be made available to navigators, physician offices, health systems, social service agencies, and others who work with Medicaid enrollees. |
| 3. | Include correct denial details. The denial letters families get do not explain the reason for denial in plain language and sometimes include incorrect reasons for denial. This makes it difficult for families to determine if they filled out the form incorrectly, or if they truly no longer qualify for coverage. |
| 4. | Share other coverage options. While Michigan’s current denial letters include information about how to reapply for Medicaid, they do not include information about other forms of health care coverage that individuals could obtain. Including plain language instructions in denial letters that outline how to apply for other healthcare coverage, including instructions on how to connect with a certified Marketplace Navigator, should be a priority. It is to our advantage as a state to ensure continuous coverage whenever possible. |
| 5. | Improve telephonic support.* While MDHHS has taken actions to address long wait times for clients calling the Universal Case Load call center, callers continue to report challenges with the long automated menu of options, delays connecting to operators who speak their native language, and dropped calls. Reporting monthly on wait times, call disconnects, and problems resolved would be a great way to ensure that the progress that’s been made continues. |
| 6. | Provide MIBridges access support. Users of MI Bridges often struggle to access their accounts. Usernames and passwords are misplaced or forgotten, and multiple failed logins leave users with locked accounts. Account recovery is difficult for users without a consistent email address. And if you contact the phone number listed, and can get connected with someone in a reasonable timeframe, the staff are often unable to help unlock accounts. |
| 7. | Offer alternative ID verification. MI Bridges requires users to verify their identity before they can access their account to update their address or complete a renewal. This is smart. But MI Bridges uses Experian for this process, which asks users to confirm information about their financial history. Many users, disproportionately unhoused Michiganders and immigrants, do not have a credit history with Experian or cannot remember the answers to the often obscure questions. There are other ways to prove identity. |
| 8. | Simplify the address change process. For Medicaid participants, having an up-to-date mailing address is critical for receiving important Medicaid renewal notices and requests for information. In MI Bridges, however, the process of changing a beneficiary’s address is confusing and duplicative. This process must be simplified. |
| 9. | Support navigators. The community based organizations that are helping Medicaid beneficiaries navigate the redetermination process are doing as much as they can to stem the losses. To ensure that residents who are eligible to retain their coverage do so and to avoid the financial consequences of dramatic insurance losses and churning, find ways to support Michigan’s navigators such as the Genesee Health Plan, the Washtenaw Health Project, etc. |
| 10. | Improve reporting. While Michigan is reporting the basic data required by CMS, the state is not reporting the data required by the Consolidated Appropriations Act, which could result in significant financial consequences for the state. Additional reporting requirements include more detail about those whose coverage has been terminated as well as information about call center volume, wait times, and abandonment rates. |
| 11. | Work with MIBridges Partners. Establish regular communication channels between MDHHS and MIBridges Partners (many of whom are community based organizations) to ensure that partners have up-to-date information and are aware of the latest changes to MI Bridges and caseworker processes (e.g. mailing list, quarterly meetings, webinars). Provide MIBridges Partners with access codes to ensure they have immediate access to caseworkers, which can serve to lighten MDHHS’ load. |
| 12. | Provide one form per household. Many heads of household receive multiple letters and forms, but do not know which family member they are being asked to renew because the forms are not labeled. In fact, if properly labeled, one form would suffice for all family members, saving the cost of mailing multiple forms and reviewing separate forms for each family member. We understand that MDHHS is attempting to implement this now, but we wish to reiterate the importance of doing so as quickly as possible. |
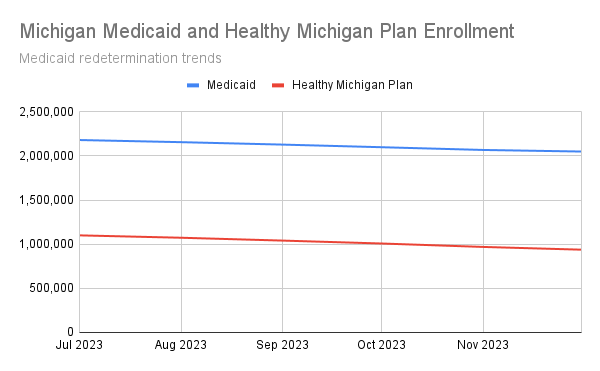
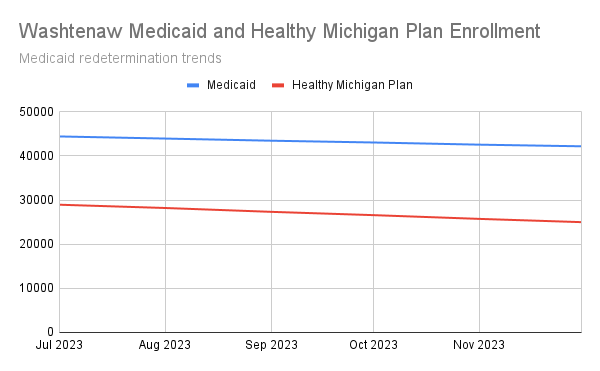
Medicaid redetermination trends