The Washtenaw Health Initiative: 2015-2017 Plan and Description
MISSION
The mission of the WHI is to improve health and healthcare in Washtenaw County with an emphasis on the low income, uninsured and underinsured[1] populations.
The WHI brings together organizations to:
- Generate innovative ideas to improve health and healthcare in the county
- Identify and share information on gaps and opportunities
- Coordinate and leverage resources
SCOPE
WHI projects meet all of the following criteria:
- Addresses an identified gap or unmet need;
- Has a primary need for planning and/or strategic direction;
- Requires multi-organization coordination and/or effort;
- Is not in the purview of another entity or where that entity requests WHI leadership;
- Where possible, has clearly defined program goals or outcome measures;
- Aligns with the goals of the WHI, listed below.
GOALS[2]
With a primary focus on the low income, uninsured, and underinsured people within Washtenaw County:
- Increase insurance coverage of uninsured individuals.
- Help those with Medicaid coverage and/or those who are underinsured maintain that coverage, understand it, use it more effectively, and/or find access to care.
- Improve coordination and integration for health care services.
- Align entities engaged in delivery of health-related services to more efficiently and effectively utilize resources.
- Strengthen community wide efforts to improve care and services for mental health and other select health issues and/or select populations.
MEASURES OF SUCCESS
- For Goal 1:
Reduce the uninsured rate among all Washtenaw County residents age 0-64 from 8.1%[3] to 4.3% (Data source: American Community Survey)
- For Goal 2:
2a – Increase the proportion of residents with an identified usual source of primary care from 84.3% to 90.2% (Data source: Michigan Behavioral Risk Factor Surveillance System)
2b – TBD measure on primary care
- For Goal 3:
Document increased effectiveness and efficiency of programs by WHI charter signatories through alignment and coordination (Data source: Survey of WHI participant organizations)
- For Goal 4:
Demonstrate perceived usefulness of the WHI through continued member participation by tracking the following process measures:
- Expand membership to include business and faith communities
- Number of members in the stakeholders group
- Number of members in attendance at quarterly WHI stakeholders meetings
- Number of WHI spinoff activities
- Number of hours volunteered by members
- Increase number of WHI charter organizations from 44 to 60
(Data source: Survey of WHI participant organizations and program data)
- For Goal 5:
Ensure that every project undertaken by the WHI will have strategic and meaningful SMART[4] goals at the outset, an evaluation plan, and an opportunity to contribute results to the continuous learning of the WHI (Data source: survey of WHI implementation leads)
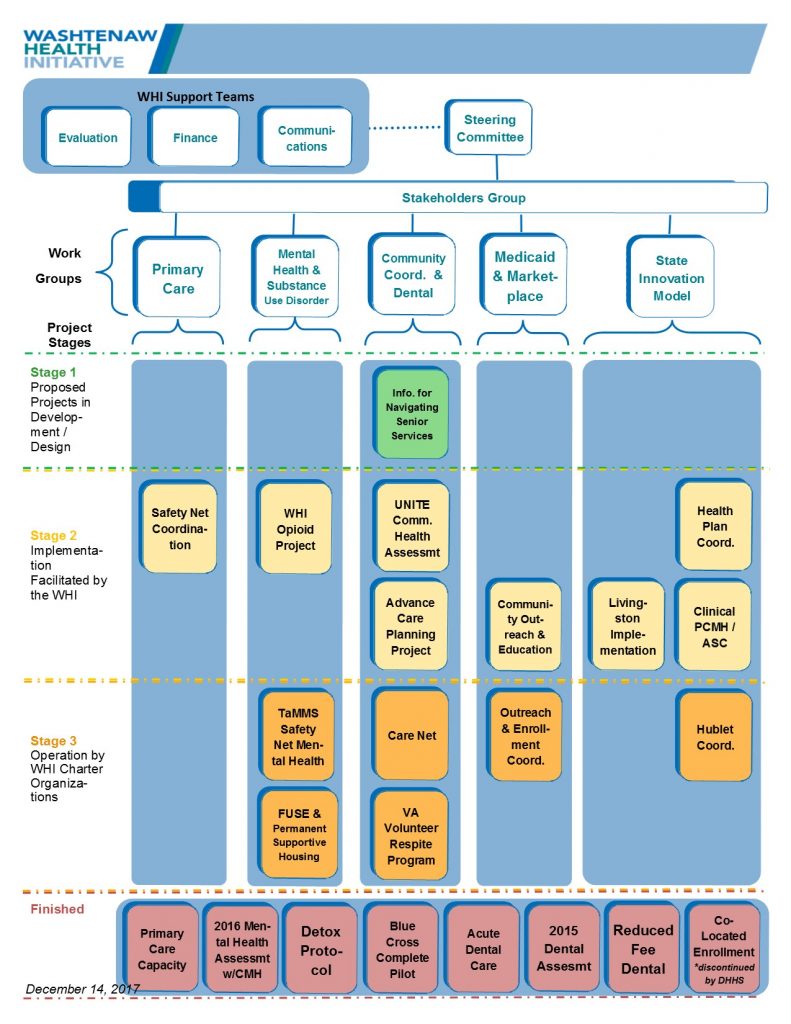
APPROACH AND ORGANIZATIONAL STRUCTURE
The WHI takes a collective impact approach to improving health and healthcare in Washtenaw County, with a special emphasis on the low income, uninsured and underinsured populations. WHI members work together on specific projects and functions with a long-term commitment to a common agenda, shared measures of success, and effective community engagement strategies.
The WHI is a voluntary collaboration of cross-sector stakeholders. The WHI is not a separate legal entity, but it does have a formal structure with clearly defined roles. There are three major groups, detailed below, that involved in carrying out the work of the WHI.
LEADERSHIP AND MEMBERSHIP PROCESSES
As a voluntary organization, WHI does not have a formal, legal structure in place. But as we look back on our progress to date and to future initiatives, it is timely to clarify the informal process of selecting members to serve on WHI’s key components. Since its inception, WHI’s structure has included the Steering Committee, the Stakeholders Group, and the Work Groups. Acting as a catalyst, the Center for Healthcare Research & Transformation (CHRT), provides expert administrative, operational, and analytical support to WHI, coordinated by the WHI Project Manager.
The purpose of this memorandum is to outline a process that will ensure continuity while simultaneously allowing WHI to evolve naturally to effectively represent the community and our constituent membership. To facilitate WHI’s sustainability, it is important to solicit feedback and support from our members in the selection process. In keeping with WHI’s informal structure and operations, the entire process will be based on consensus rather than a formal voting process. What follows is the Steering Committee’s recommended structural and operational approach.
The Steering Committee
The Steering Committee provides strategic oversight and sets program priorities. Every three years, the Steering Committee will assess what, if any, changes need to be made to Steering Committee membership. In addition, the Steering Committee will also review the structure and composition of the WHI overall. The Steering Committee consists of no more than 22 members divided into two groups, Organizational and Community members. The groups are not required to be equal in size. The Steering Committee Roles tables below show the proposed arrangement.
Organizational Members. One group consists of members representing, at present, eight specific organizations that remain essential to WHI’s mission. For this group, the organization will designate its Steering Committee representative, who will serve until the organization chooses to select another representative. Because we anticipate a reasonable amount of individual turnover, we do not recommend staggered terms at this point.
This process allows the Steering Committee to adjust for changes in which organizations are designated as permanent members. As WHI’s initiatives change over time, new organizations may become increasingly integral to Steering Committee activities. When that occurs, the Steering Committee may add an organization or replace an organization whose emphasis may have shifted away from WHI’s mission.
Community Members. The second group consists of community-based members who will represent sectors with many organizations that could contribute to the Steering Committee, such as the business and philanthropic sectors. Thus, these members will serve rotating, three-year terms, renewable up to three times. Currently, there are nine community-based representatives— some members unaffiliated with a specific organization, one academic member, one business community member, and one member representing a local philanthropy.
In this category, we anticipate having at least five members from the community, including local businesses. The Steering Committee will select two of those members as WHI Co-Chairs. To recruit community-based members, the Steering Committee will consult with the Stakeholders Group to ensure a collaborative process in identifying WHI’s leadership.
Organizational Positions as of December, 2017
| Organizational Role | Current Member | Current Member Title & Organization |
| 1. Community Mental Health Director | Trish Cortes | Director, Washtenaw Community Mental Health |
| 2. IHA Representative | Dr. Marti Walsh | Chief Quality and Population Health Officer, Integrated Health Associates |
| 3. Livingston County Representative | Connie Conklin | Community Mental Health Services of Livingston County |
| 4. Washtenaw County Public Health Department Director | Ellen Rabinowitz | Public Health Officer, Washtenaw County Public Health; Executive Director, Washtenaw Health Plan |
| 5. SJMHS-Ann Arbor Executive | David Brooks | President and Chief Executive Officer, St. Joseph Mercy Ann Arbor and Livingston |
| 6. SJMHS-Ann Arbor Clinical | Rosalie Tocco-Bradley | Chief Medical Officer, St. Joseph Mercy Ann Arbor and Livingston |
| 7. SJMHS-Chelsea Executive | Nancy Graebner | President and Chief Executive Officer, St. Joseph Mercy Chelsea |
| 8. UMHS Executive | Tony Denton | Senior Vice President and Chief Operating Officer for University of Michigan Hospitals, Health Centers, and Medical Group |
| 9. UMHS Clinical | Brent Williams | Associate Professor of Internal Medicine, Michigan Medicine |
| 10. VA Ann Arbor Healthcare System Executive | Open | Open |
| 11. VA Ann Arbor Healthcare System Clinical | Leo Greenstone | Associate Chief of Staff for Ambulatory Care, VA Ann Arbor Healthcare System |
Community Positions as of December, 2017
| Community Member Role | Current Member | Current Member Title & Organization | WHI Steering Committee Term |
| 12. Community Representative | Jack Billi | Professor, Internal Medicine and Health Management and Policy, University of Michigan | 6/2015 – 5/2018 |
| 13. Community Representative | Ann Davis | Retired Administrator, Chelsea Community Hospital | 6/2015 – 5/2018 |
| 14. Community Representative* | Bob Guenzel | Retired County Administrator | 1/2015 – 12/2017 |
| 15. Community Representative* | Norman Herbert* | Retired Treasurer, University of Michigan | 1/2015 – 12/2017 |
| 16. Community Representative | Pastor George W. Waddles | Second Baptist Church, Ypsilanti | 9/2017 – 8/2020 |
| 17. Community Representative | Doug Strong* | Retired Chief Executive Officer, Michigan Medicine | 6/2015 – 5/2018 |
| 18. Community Representative – Business | David Sarns | 360 Advisors, L.L.C. | 6/2015 – 5/2018 |
| 19. Community Representative | Gregory Dill | County Administrator, Washtenaw County | 11/2017 – 10/2020 |
| 20. Academic | Peter Jacobson | Professor of Health Law and Policy; Director of the U-M Center for Law, Ethics, and Health, University of Michigan School of Public Health | 1/2015 – 12/2017 |
| 21. Philanthropic Organization Representative | Pam Smith | President and Chief Executive Officer, United Way of Washtenaw County; Member, Coordinated Funders | 1/2015 – 12/2017 |
| 22. Community Representative | Open |
* Denotes WHI co-chair
The Steering Committee may have up to 22 total members at the discretion of the Steering Committee.
Work Group Chairs as of December, 2017
| Ex Officio (Non-Voting) Position | Current Member | Current Member Title & Organization |
| 1. Community Coordination Work Group Chair | Ruth Kraut | Program Administrator, Washtenaw Health Plan |
| 2. Communications Work Group Chair | Liz Conlin | Account Director, re:group |
| 3. Medicaid & Marketplace Outreach & Enrollment Work Group Chair | Cindy Bodewes | Senior Director Patient Business Services, Michigan Medicine |
| 4. Mental Health & Substance Use Disorder Work Group Co-Chair | Gregory Dalack | Psychiatry Department Chair, Michigan Medicine |
| 5. Mental Health & Substance Use Disorder Work Group Co-Chair | Nancy Siegrist | Director of Behavioral Health Services, St. Joseph Mercy Chelsea |
| 6. Primary Care Work Group Co-Chair | Brandie Hagaman | Program Administrator of Health Services Innovations, Community Support & Treatment Services |
| 7. Primary Care Work Group Co-Chair | Mark Jacoby | Practice Administrator, Packard Health |
| 8. State Innovation Model Work Group Co-Chair | Paul Valenstein | President, St. Joseph Mercy Partners Clinically Integrated Network |
| 9. State Innovation Model Work Group Co-Chair | Doug Strong | Retired Chief Executive Officer, Michigan Medicine |
Stakeholders Group
The Stakeholders Group consists of local individuals, community-based organizations, and governmental agencies that share WHI’s mission and goals. As a collaborative endeavor, WHI welcomes individuals and entities willing to sign the Charter (below), setting forth the 2015-2017 Statement of Commitment. WHI also welcomes other guests at the Stakeholders Group quarterly meetings.
A key role for the Stakeholders Group is to provide feedback on WHI’s strategic direction and to participate in projects. WHI relies on the Stakeholders Group to identify areas related to WHI’s mission that Work Groups should address.
Although the Steering Committee will have initial responsibility for selecting its membership, the recommendations will be submitted to the Stakeholders Group for input. The Stakeholders Group will also have the opportunity to suggest new organizations that should be represented on the Steering Committee.
Work Groups
The implementation of WHI’s strategic vision occurs through various Work Groups. The Work Groups are organized around themes to improve health and health care for uninsured and underinsured populations, such as access to primary care, mental health, and Medicaid outreach and enrollment. Under the direction of a Work Group Chair or Co-Chairs, each theme involves several different projects.
The charge of the Work Groups is to share information among WHI member organizations in the theme area, identify gaps in the community that fall into that theme area, develop new projects to address those gaps, and monitor those projects. Work Groups usually meet between 4-12 times per year
The Work Group Chair/s is/are selected for his or her expertise in the theme area. The Steering Committee will designate the Work Group Chairs. Chairs agree to serve for a term of two years, renewable based upon mutual agreement with the Steering Committee leadership.
A significant aspect of the Work Group process is the opportunity to engage various segments of the WHI membership, along with community groups that are not WHI members. For instance, projects that directly involve government processes and policies, such as Medicaid outreach and enrollment, can benefit from including governmental officials as participants. Likewise, the projects can include consumer representatives with lived experiences in the various topics being addressed.
[1] Underinsured individuals are those who have incomes below 250% of the Federal Poverty Level guidelines, and either: 1) have an unaffordable plan with high co-pays and deductibles; or 2) require medically necessary services not covered under their Medicaid or their private plan.
[2] The goals of the WHI are not hierarchical, nor are they mutually exclusive; WHI projects may be focused on achieving more than one, or all, of the WHI’s goals.
[3] Among the civilian non-institutionalized population using 2011-2013 American Community Survey 3-Year estimates.
[4] SMART goals are those that are specific, measurable, achievable, realistic, and time-bound. Source: CDC Communities of Practice – http://www.cdc.gov/phcommunities/resourcekit/evaluate/smart_objectives.html